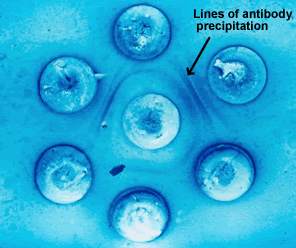
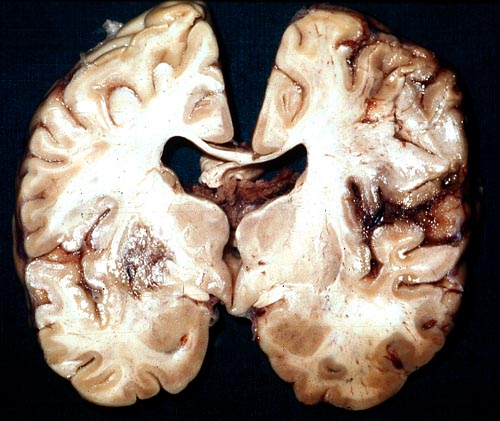
Cerebral Aspergillosis – Gross PathologySection though unfixed brain showing large pale area of infarction deep in the parietal cortex, in which Aspergillus sp. hyphae were seen histologically. The patient developed disseminated aspergillosis after a prolonged stay in intensive care after contracting severe community acquired pneumonia. |
 |
||
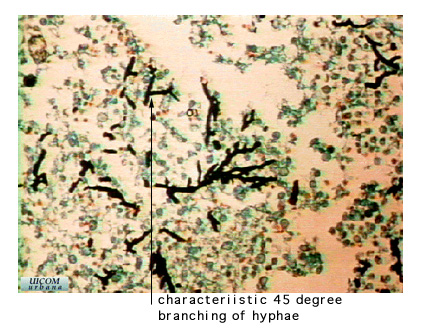
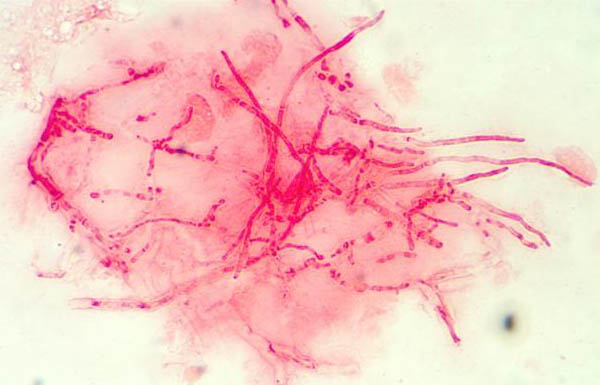
Lung, Aspergillus InfectionAspergillus is an opportunistic fungus. It is an ascomycete and therefore is characterized by dimorphism (yeast forms and hyphae forms), septate hyphae, sexual spores found in an ascus and asexual spores (conidia) found on conidiophores. Aspergillus can be identified quickly by its septated hyphae and the 45 degree angle branching of its hyphae. |
 |
||
|
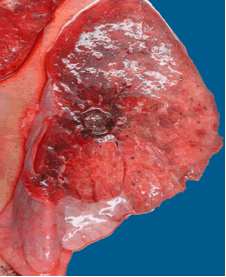
Aspergillus niger - Fungal ball Gross section of lung at autopsy showing a discrete, well-demarcated dark/black mass surrounded by a fibrotic capsule. No evidence of local invasion, or infarction. The patient had had acute myeloid leukaemia (M1) and responded poorly to chemotherapy. He developed A.niger endocarditis and disseminated disease to the kidneys, lumbar disc and heart, probably arising from this lesion. It is unclear whether this lung lesion was a partially cured ‘mycotic lung sequestrum’ following antifungal therapy, or originated as an aspergilloma. The confirmation of genus and species was obtained by PCR on blood and vegetations. |
 |
||
|
Lung, Aspergillosis Arrow one indicates a conidiophore which is the stalk which supports a conidia as seen at arrow 2. The conidia are the spores of the ascomycete. The conidiophore and the conidia are part of the asexual stage of the life cycle of the ascomycete. Arrow 3 highlights a hypha. No septae are visible in this example. Arrow 4 shows a mycelium which is in a mat of hyphae.
|
 |
||
Sphenoid Sinusitis in AIDSBase of skull at autopsy showing pus in the sphenoid sinus and destruction of the lateral wall of the sinus, as demonstrated on the CT scan. Cultures from the sinus and brain abscess grew Aspergillus fumigatus
|
 |
||
|
Allergic Fungal Sinusitis Also as eosinophilic fungal rhinosinusitis, light microscopy of mucus sections. Histological sections of formalin fixed and paraffin embedded mucus, from patients suffering from allergic fungal sinusitis (eosinophilic fungal rhinosinusitis). Kindly provided by Jens Ponikau, Mayo Clinic. Copyright Mayo Foundation 2003
|
 |
||
MRI Fungal SinusitusCalicifications in imaging. Allergic fungal sinusitis (AFS) is commonly caused by Aspergillus. Patients often have associated asthma. The MRI in addition to radiological abnormalities, thick pus or a clay-like substance was found in the sinuses. There was no allergic mucin, but dense hyphae are found. An inflammatory response in the mucosa was noted.. Upon looking into the sinus, the fungus ball can vary in size from 1 mm or smaller to a size which completely occupies the sinus. It may have a greenish-black appearance. Removal of the fungus ball is the typical treatment. |
 |
||
|
Corneal Ulcer - Gram Stain Corneal scrapings were taken from a 67 yr old farmer presenting with a corneal ulcer of the right eye. A piece of vegetable matter was embedded in the cornea and scrapings were done. Gram stain (500x magnification) showed numerous septate hyphae. Cultures grew a small amount of A fumigatus Kindly provided by Dr Ken Stottler (© Fungal Research Trust)
|
 |
||
Aspergillus KeratitisCase Report: A 52 year-old man was grinding a metal fire escape, which was overgrown with creepers. Two days later, he attended his local eye unit for the removal of metallic corneal foreign body from the left eye, the site of which became infected and subsequently unresponsive to topical antibiotic. Eleven days after the injury, Aspergillus fumigatus was grown from a corneal scrape. Despite topical amphotericin and referral to a regional centre where systemic Itraconazole was added, the keratitis continued to worsen, becoming severely painful, requiring systemic opiates. A penetrating corneal graft with intraocular amphotericin was performed 6 weeks after the injury, under general anaesthesia. Systemic treatment was continued and monitored by the regional Infectious Disease Department for a further 2 months after surgery; the patient is making good progress with near normal vision, 9 months after surgery. NB: Photograph was taken 5 weeks after the injury. |
 |
||
|
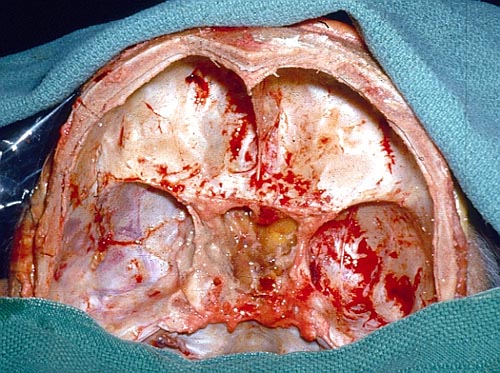
Endocarditis Macroscopic view of the heart at autopsy, showing an infracted lesion on the papillary muscle of the mitral valve in the left ventricle. In addition the patient had large vegetations, which are not shown here. The confirmation of genus and species was obtained by PCR on blood and vegetations; the pericarditis was a manifestation of disseminated aspergillosis. Reported in association with with infection of long-standing central venous catheters.
|
 |
||
|
Chest X-Ray - Enocarditis Diagnosis This (normal) chest X-ray was taken about 6 weeks before endocarditis was diagnosed, and 3 months before death due to disseminated aspergillosis. No CT scan was done (a chest radiograph has a 10% false negative rate in leukaemic patients, compared with CT) |
 |
||
|
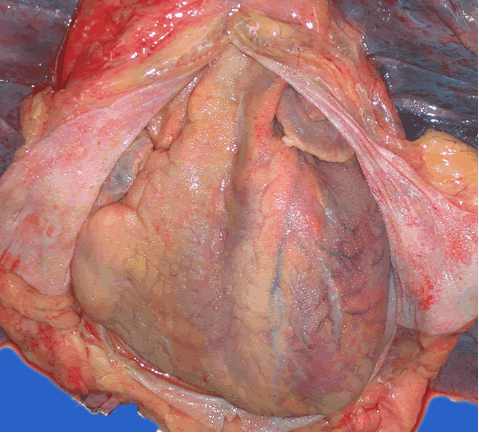
Pericardits - Aspergillus niger Myocarditis and pericarditis are complications of disseminated disease. Macroscopic view of the pericardium at autopsy, showing gross chronic haemorrhagic pericarditis. The confirmation of genus and species was obtained by PCR on blood and vegetations; the pericarditis was a manifestation of disseminated aspergillosis. Three patients have been reported to have survived when treated. One with amphotericin B and the other two with Itraconazole. |
 |
||
|
Lumbar Discitis Macroscopic lesion of a lumbar intervertebral vertebral at autopsy, showing haemorrhagic necrosis, caused by hyphal invasion and infarction. The confirmation of genus and species was obtained by PCR on blood and vegetations; the discitis was a manifestation of disseminated aspergillosis. Submitted by Dr R. Barnes and Dr C. Poynton, Cardiff.
|
 | ||
Wound Mycotic InfectionThis patient, (whose case is presented in Carlson et al, J Infect 1996;33:119) had had a laparostomy for recurrent intra-abdominal sepsis following on from Crohns disease. She was transferred to another intensive care unit and her dressings changed daily. Shortly after, this dark patches appeared on her liver (as seen here) and her colon. Superficial biopsies and culture showed Aspergillus fumigatus invading liver capsule. She responded to amphotericin B therapy. |
 |
||
|
Neonatal Primary Cutaneous Aspergillosis – Buttocks Lesion Neonatal primary cutaneous aspergillosis usually presents as an erythematous plaque with pustules that evolve into an eschar. Immunocompromised patients and premature neonates are at risk of developing this disease. Early diagnosis and treatment are critical in preventing progression to a systemic illness. Woodruff CA, et al. Pediatr Dermatol 2002;5:439-44. |
 |
||
| Aspergillus
sp. Infection of burn wound
This photo shows
extensive infection of the burn wound on the leg of a 7 year
old boy, acquired about 3 weeks after the injury. Despite
medical therapy he died
|
 |
||
Aspergillus onychomycosisAlthough Candida sp. yeast infections are common in onychomycosis, in this case was caused by Aspergillus terreus known to be resistant to AMB.
|
 |
||
|
Aspergillus onychomycosis Onychomycosis caused by Aspergillus fumigatus
|
 |
||
|
Double Diffusion test for Aspergillosis. Central well contains Aspergillus fumigatus antigen and wells in the top and bottom contain control antiserum. The three peripherals wells with precipitin bands contain sera from patients with A. fumigatus fungus ball (FB). More bands present in the upper right cases is characteristic of FB. The well in the bottom left position is negative. Images supplied by LC Severo, with the help of AC Pasqualotto, at Santa Casa Complexo Hospitalar, Porto Alegre, Brazil |
|||